Pneumonia is an infection of the lungs most often caused by a virus or bacteria. What are the causes of the disease? How is it diagnosed?
Find out everything you need to know in this sheet.
Pneumonia, what is it?
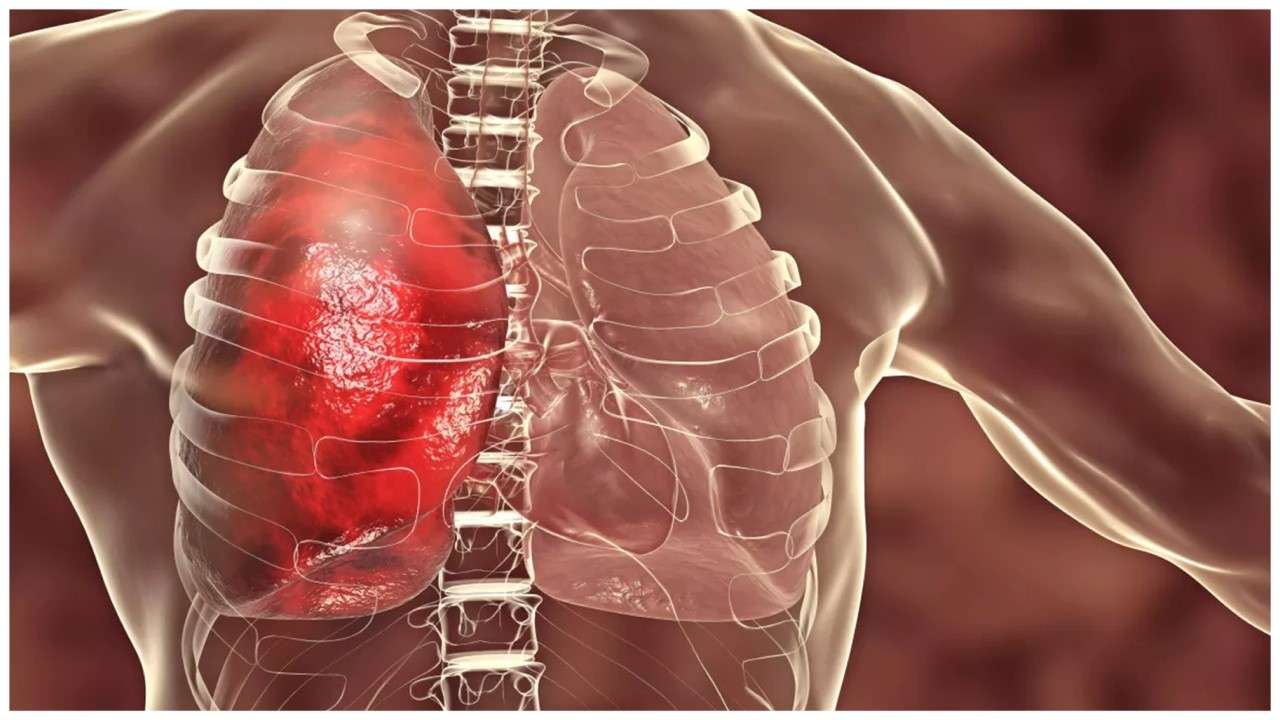
Pneumonia is an infection of the lungs most often caused by a virus or bacteria.
The infection more specifically affects the alveoli, these tiny bags in the shape of balloons located at the end of the bronchioles (see the diagram below). It usually affects only one of the 5 lobes of the lung (3 lobes in the right lung and 2 in the left), hence the term lobar pneumonia. When pneumonia also affects the bronchi, it is called bronchopneumonia.
Pneumonia actually refers to a wide variety of infections that can be mild or life threatening. Thus, if pneumonia appears as a complication of a serious illness or in an elderly person, it can be fatal. In very rare cases, pneumonia can also be fatal in a healthy person.
The disease is usually manifested by a cough often accompanied by sputum, shortness of breath, fever and chills. Pneumonia is most often caught like the flu or a cold, by inhaling contaminated particles. In some cases, it occurs after another respiratory infection, such as the flu or bronchitis, which « degenerates » and settles in the alveoli of the lungs. Some of the symptoms can last for several weeks. It is usually not very contagious.
The term pneumonia is sometimes used as a synonym for pneumonia. In fact, in medical usage, pneumonia refers to an infection of the lungs caused by a microbe (virus, bacteria), while pneumonia is a broader term meaning « lung disease ». There are, for example, forms of pneumopathy caused not by microbes, but by the inhalation of irritating products, dust or prolonged use of tobacco. Their symptoms resemble those of pneumonia.
What causes pneumonia?
Almost all pneumonia is caused by germs, viruses or bacteria. When the microbe attacks the lungs, the body responds by triggering an inflammation response. The alveoli fill with pus and inflammatory fluid, which leads to breathing difficulties.
The doctor must make a distinction between two modes of pneumonia contraction: contraction in a hospital environment (nosocomial pneumonia) and contraction outside the hospital (community-acquired or “community-acquired” pneumonia). Nosocomial pneumonias are generally more dangerous, as they occur in people weakened by another disease. In the hospital, pneumonia is often transmitted by mechanical ventilation devices (intubation) in intensive care units.
The exact type of bacteria or virus responsible for pneumonia in a given patient is only known in half of the cases , in part because laboratory techniques are not efficient enough. For your information, here are the ones most commonly found in people with pneumonia.
Bacteria that cause pneumonia
Bacterial infections most often cause typical pneumonia. Most of the time, the bacteria Haemophilus influenzae, Staphylococcus aureus or Streptococcus pneumoniae (causing pneumococcal pneumonia), are responsible.
Atypical pneumonia
It manifests with symptoms that may be less pronounced than typical pneumonia. For example, some people with pneumonia have no fever or chest pain. Pneumonia then suggests a respiratory infection, such as bronchitis, sinusitis or the flu (influenza).
Among the bacteria that cause atypical pneumonia are Mycoplasma pneumoniae (causing mycoplasma pneumonia), Chlamydia pneumoniae and Legionella pneumophila (responsible for Legionnaire’s disease).
The viruses involved
The most common viruses responsible for pneumonia are influenza and parainfluenza viruses, respiratory syncytial virus, cold viruses (rhinovirus), herpes-type viruses or the SARS virus. The influenza virus, that is to say that of the flu, sometimes reaches the pulmonary alveoli and thus causes viral pneumonia. Subsequently, the respiratory system weakened by the viral infection can open the door to a potentially more serious bacterial superinfection.
At the beginning of 2003, an epidemic of SARS or severe acute respiratory syndrome claimed victims in several countries. China, Singapore and Canada (especially the city of Toronto) were the most affected. In total, more than 8,000 people were then infected with SARS. Of these, 800 died, including 43 in Canada . The epidemic was brought under control within 4 months thanks to measures aimed at preventing its transmission (wearing of masks, quarantine, etc.). SARS is caused by a highly contagious coronavirus.
Other rarer causes of pneumonia
Aspiration pneumonia
It occurs when some of the liquid in the stomach is sucked into the lungs. The bacteria present in this liquid then reach the bronchi and the alveoli of the lungs and cause an infection. This phenomenon generally occurs after anesthesia or following a neurological disorder affecting the swallowing reflex or in case of inhalation of vomiting, due to overconsumption of alcohol or drugs.
Inhalation of toxic products
inhalation of certain toxic products (kerosene, varnish, paint thinner, etc.) or mold (during construction work, mainly in people whose immune system is weakened by immunosuppressive treatment), or an allergy to products used in the workplace can cause inflammation of the lungs and bleeding. These conditions increase the risk of pneumonia and can cause pneumonitis, inflammation of the lungs, of non-infectious origin.
Tuberculosis
Tuberculosis can present as pneumonia.
The weakened immune system
Pneumonia caused by a parasite or fungus is most common in people with weakened immune systems. Pulmonary aspergillosis is an example, as is pneumocystosis (caused by a parasite).
Who is affected by pneumonia?
According to the World Health Organization, in 2015, pneumonia was responsible for 15% of deaths among children under 5 years old. It is therefore a dangerous disease in young children, which is why the WHO recommends vaccination to prevent pneumonia.
According to the Quebec Lung Association, 200,000 to 300,000 Canadians suffer from pneumonia each year and the mortality rate can reach 30% in certain populations (elderly people – over 65 -, hospitalized, etc.). Hospital-acquired pneumonia affects 0.5% to 1% of hospitalized patients, but up to 40% of people on mechanical ventilation in intensive care 17 .
Consult our article on people at risk.
Diagnosis: how do you recognize pneumonia?
The doctor evaluates the symptoms, inquires about the family history and auscultates the lungs. He can order an x-ray examination of the lungs and ask for an analysis of the pulmonary secretions (expelled by coughing). If necessary, he will resort to other tests, for example the search for bacteria in the blood.
See in detail the symptoms of pneumonia.
What are the complications of pneumonia?
Pneumonia is usually cured in 2 weeks or a little more. However, more time is often needed before full recovery.
Although rare, some serious complications are possible:
A pleural effusion
It is the accumulation of inflammatory fluid between the two layers of the pleura that causes compression of the lung. If there is a lot of liquid, it must be removed by suction. Exceptionally, it happens that this liquid persists and becomes purulent. Surgery is then often necessary.
Respiratory distress
When pneumonia affects both lungs, breathing becomes extremely difficult. Assisted ventilation is then often necessary.
A septic shock
That is to say a generalized infection of the body due to the passage of the bacteria from the lungs to the blood. This occurs especially with pneumococcal pneumonia.
Other
- a lung abscess.
Thanks to antibiotics, pneumonia causes far fewer deaths than before. Still, pneumonia and the flu (influenza) together are the leading cause of death from an infectious disease in Canada. The very old, with weaker immune systems, and people with other serious illnesses are most likely to succumb to it.
Read « pneumonia treatments »
Pneumonia can be recognized by a sudden rise in fever of up to 41ºC (106ºF), but this is not the only symptom of this infectious lung disease.
Check out the full list below.
Symptoms of pneumonia
Typical pneumonia
- A sudden rise in fever up to 41 ºC (106 ºF) and severe chills;
- shortness of breath, rapid breathing and pulse;
- a cough. At first, the cough is dry. After a few days, it becomes greasy and is accompanied by yellowish or greenish secretions, sometimes streaked with blood;
- chest pain that intensifies during coughing and deep inspirations;
- deterioration in general condition (fatigue, loss of appetite);
- muscle pain;
- headaches ;
- wheezing.
Certain serious signs should lead to immediate hospitalization:
- altered consciousness;
- pulse too fast (greater than 120 beats per minute) or respiratory rate greater than 30 breaths per minute;
- temperature above 40°C (104°F) or below 35°C (95°F).
Atypical pneumonia
“Atypical” pneumonias are more misleading because their symptoms are less specific.
They can be manifested by headaches, digestive disorders or joint pain. Cough is present in 80% of cases, but in only 60% of cases in the elderly.
People at risk are most often children, the elderly, people with chronic respiratory disease, etc.
But do you know the risk factors for this disease?
Consult them in our file.
People at risk of pneumonia
A certain population is more at risk of contracting pneumonia, while certain factors increase the risk and can be avoided.
- Children and especially young children. The risk increases more in those who are exposed to second-hand smoke;
- the elderly, especially if they live in a retirement home;
- people with chronic respiratory disease (asthma, emphysema, COPD, bronchitis, cystic fibrosis);
- people with a chronic disease that weakens the immune system, such as HIV/AIDS infection, cancer, or diabetes;
- people who receive immunosuppressive treatment or corticosteroid therapy are also at risk of suffering from opportunistic pneumonia;
- people who have just had a respiratory infection, such as the flu;
- people in hospital, in particular in an intensive care unit;
- people exposed to toxic chemicals in the course of their work (for example, varnishes or paint thinners), bird breeders, workers involved in the manufacture or processing of wool, malt and cheese ;
- Indigenous populations in Canada and Alaska are at greater risk of pneumococcal pneumonia.
Pneumonia risk factors
- Smoking and exposure to second-hand smoke;
- alcohol abuse ;
- drug use;
- substandard and overcrowded housing.
In order to prevent pneumonia, certain measures can be put in place on a daily basis, especially during the winter.
Discover the complete list of these measures in this sheet.
How to prevent pneumonia?
Basic preventive measures
- Have a healthy lifestyle (sleep, diet, physical exercise, etc.), especially during the winter. Consult our Strengthening your immune system sheet to find out more;
- not smoking helps prevent pneumonia. Smoke makes the airways more vulnerable to infection. Children are particularly sensitive to it;
- wash your hands regularly with soap and water, or with an alcohol-based solution. Hands are constantly in contact with germs that can cause all kinds of infections, including pneumonia. These enter the body when one rubs one’s eyes or nose and when one brings one’s hands to one’s mouth;
- when taking antibiotics to treat an infection, it is important to follow the treatment from start to finish;
- respect the hygiene measures displayed in clinics and hospitals such as washing hands or wearing a mask, if necessary.
Other measures to prevent the onset of the disease
Vaccine against influenza
The influenza virus can cause pneumonia directly or indirectly. Thus, the flu vaccine reduces the risk of pneumonia. It must be renewed every year.
Specific vaccines
The pneumococcal vaccine protects with variable effectiveness against pneumonia due to Streptococcus pneumoniae, the most frequent in adults (it fights 23 serotypes of pneumococci). This vaccine (Pneumovax®, Pneumo® and Pnu-Immune®) is mainly indicated for adults with diabetes or COPD, people with weakened immune systems and those aged 65 and over.
Its effectiveness has been convincingly demonstrated in the elderly who reside in long-term care centres. The Prévenar® vaccine offers good protection against meningitis in young children, and slight protection against otitis and pneumonia caused by pneumococcus. The Canadian National Advisory Committee on Immunization recommends its routine administration to all children 23 months or younger to prevent meningitis. Older children (24 months to 59 months) can also be vaccinated if they are at high risk of infection.
The American Academy of Pediatrics also recommends this vaccination. In Canada, routine vaccination against Haemophilus influenza type B (Hib) is recommended for all infants from 2 months of age. Three conjugate vaccines are licensed in Canada: HbOC, PRP-T and PRP-OMP. The number of doses varies according to age at first dose.
Measures to promote healing and prevent worsening
First of all, it is important to respect a rest period.
Throughout illness, avoid exposure to smoke, cold air, and air pollutants as much as possible.
Measures to prevent complications
If the symptoms of pneumonia persist with the same intensity 3 days after the start of antibiotic treatment, you should see your doctor as soon as possible.
The treatment depends above all on the cause of the pneumonia (bacteria, virus, fungus, etc.). To choose the appropriate treatment, the doctor also bases himself on the person’s age, state of health and physical examination and, if necessary, on various additional analyses.
Discover the different possible treatments in our sheet.
How to treat pneumonia?
home treatment
Bacterial pneumonia
In healthy people, most community-acquired pneumonia is treated with a macrolide antibiotic (erythromycin, clarithromycin, azithromycin). There is usually no reason to go to the hospital.
The bacteria responsible for pneumonia are increasingly resistant to antibiotics. The phenomenon is particularly worrying in the case of pneumonia acquired in hospital. If the antibiotic does not seem to be working after a few days, it may be necessary to change the antibiotic. To avoid contributing to resistance, it is important to complete your treatment as prescribed by your doctor.
viral pneumonia
Most of the time, viral pneumonias heal without treatment. Antibiotics are not effective against viruses. In some cases, antiviral medications may be used, such as oseltamivir (Tamiflu®) or zanamivir (Relenza®). If necessary, other medications will help relieve chest pain and lower fever (paracetamol, also called acetaminophen, and more rarely ibuprofen, which is more recommended in Quebec).
As for the cough, it should not be completely eliminated since it helps to expel the secretions that clog the bronchi. Cough syrups are also generally discouraged by doctors. To relieve coughs and sore throats, natural solutions, such as drinking hot water to which a little honey has been added, are preferable.
Respiratory physiotherapy
This technique, especially used in people with a chronic respiratory disease, can help unclog the airways. In Quebec, respiratory therapists teach it to patients. Percussion movements are performed on the patient’s back, which triggers coughing and evacuates secretions. The person should be lying on their stomach with their upper body tilted down. Chest physiotherapy appears to help shorten healing time and prevent complications.
Followed
A visit to the doctor, 4 to 6 weeks after the diagnosis and a chest X-ray will make sure that the pneumonia is well cured. If it does not heal within the usual time, the doctor will recommend an appropriate investigation, such as a CT scan or a bronchoscopy. Persistent pneumonia can be caused by a tumor in a bronchus.
Hospital treatment
When pneumonia is severe or the risk of complications is high, hospitalization may be necessary. Drugs can then be administered intravenously or even oxygen supplied if the blood oxygen level is found to be too low. Most people hospitalized with pneumonia are babies, young children, the elderly, or people who are debilitated and have chronic illnesses.
For better comfort
- The seated position is the most comfortable. Horizontally, breathing is more labored. At night, opt for a slightly reclined position. Elevate the back with pillows;
- applying a warm, moist compress to the chest helps relieve chest pain;
- stay well hydrated;
- in the early stages of the disease, avoid exposure to cold air;
- stop strenuous physical activities. Resume them gradually, according to abilities;
- do not take cough syrup without asking the doctor’s advice. Some over-the-counter syrups may block the passage of mucus and make the situation worse.
As part of its quality approach, Passeportsanté.net invites you to discover the opinion of a health professional.
Dr. Dominic Larose, emergency physician, gives you his opinion on pneumonia.
Dr. Dominic Larose’s opinion on pneumonia
« Pneumonia is very common, and has many faces. On the one hand, an uncomplicated recovery can be expected in the majority of cases (with medical treatment), but on the other hand pneumonia is one of the causes among the most frequent deaths.
Indeed, it happens, but very rarely, that a young and healthy person dies of lightning pneumonia. A few exceptional cases of young people dying from viral pneumonia (influenza) have thus attracted some attention from the media. But most people who die of pneumonia are more likely to be in high-risk groups.
If you have symptoms of pneumonia, it’s best to see a doctor quickly for proper diagnosis and treatment. »
Dr. Dominic Larose MD
The unconventional treatments presented here do not cure pneumonia, but may provide comfort and relieve symptoms.
Discover all the details on these more natural methods in the sheet below.
Complementary approaches for pneumonia
The following unconventional treatments do not cure pneumonia. They can provide comfort and relief, in addition to medical treatment. Some help strengthen the body’s natural defenses. See also our Strengthening the immune system sheet.
Probiotics
Probiotics may help prevent pneumonia in children due, it is believed, to their boosting effect on the immune system.
A clinical trial3 showed that the consumption of fermented milk (Actimel®, which contains lactobacilli of the Lactobacillus casei type), reduced the incidence of lower respiratory infections (bronchitis and pneumonia). In another trial4, supplementation with Lactobacillus GG was found to provide mild but statistically significant protection against infections of the respiratory system (otitis, sinusitis, bronchitis and pneumonia)4.
If needed, other drugs will help relieve chest pain and lower fever (ibuprofen, paracetamol).
In addition, several studies suggest that probiotics could limit the risk of hospital-acquired pneumonia in patients on mechanical ventilation. A trial of 146 patients, half of whom received Lactobacillus twice a day, showed that their risk of pneumonia was reduced by 218.
Finally, taking probiotics helps prevent the diarrhea that can accompany taking antibiotics.
Consult the Probiotics sheet for more information.
Ail (Allium sativum)
Traditionally, garlic has been used to fight infections of all kinds, as well as to prevent colds and flu. ESCOP recognizes its use for treating upper respiratory tract infections, such as the common cold. The effect of garlic consumption on the symptoms of pneumonia has been tested in only a few subjects with this condition5.
Dosage: consume about 4 cloves of fresh garlic (16 g) per day, or take 2 g to 4 g of dried garlic, 3 times a day. It can also be taken as a tincture or standardized extract. See the Garlic (psn) sheet for more information.
Isatis (Isatis tincture)
In Traditional Chinese Medicine, the root of isatis (Chinese name: Ban Lan Gen) is used, in association with other plants of Chinese herbalism, to treat a multitude of ailments, including upper respiratory infections and certain pneumonias. Isatis also experienced a resurgence in popularity in 2003, in Asia, due to the SARS (severe acute respiratory syndrome) epidemic.
Several in vitro and animal tests demonstrate that isatis root, in extract form, has antibacterial and antiviral properties.
Dosage: Consult a trained practitioner of Traditional Chinese Medicine for personalized treatment.
Dietary restrictions
Naturopaths and Dr. Weil recommend avoiding certain foods that increase mucus production. Foods to banish are milk and dairy products, very sweet foods and those prepared with bleached wheat flour. But these recommendations remain a subject of controversy within the scientific community.
Steam inhalation
Inhaling steam containing German chamomile, black elderflower or lemon balm can help reduce irritation of the throat and bronchial tubes6. They also help expel secretions.
Procedure14: put 30 g of the chosen plant in 1 liter of boiling water. Remove from the heat and let steep for 15 minutes. Pour the infusion into a large bowl. Place your head above the bowl and inhale the steam for about ten minutes. Place a towel to cover the head and bowl to prevent steam from escaping. It is then recommended to stay warm for at least 30 minutes, in order to facilitate the evacuation of mucus.
Mustard poultice
Applied to the chest, the mustard poultice (also called “mustard fly”) is said to help soothe pain and reduce fever6,13. It would also stimulate the production of fluids in the lungs, facilitating the expulsion of mucus. To take full advantage of its expectorant effect, once the application is finished, you can start a respiratory physiotherapy session (see the Medical treatments section).
Preparation :
- mix 1 part dry mustard with 2 or 3 parts wheat flour;
- add a little warm water to obtain a paste;
- spread the paste on a cloth and fold it in half to avoid direct contact with the skin;
- place on the chest or on the upper back;
- leave to act for 10 to 15 minutes;
- if possible, apply twice a day.
Warning: check the temperature of the poultice before applying it to avoid burns. In some European countries, you can find ready-to-use mustard poultices in pharmacies.
relaxation techniques
Regardless of the preferred technique (deep breaths, autogenic training, biofeedback, etc.), the aim is to reduce muscle tension in order to promote healing13. You should know that people who suffer from pneumonia have chest pains that intensify during coughs and deep inspirations.
See also the Relaxation Response sheet, which describes the steps that guide the body towards relaxation. See also our guided relaxations in Meditate – and much more.
Manual lymphatic drainage
This gentle massage technique stimulates lymph circulation. This carries several components that participate in the body’s immune reactions. This is why some believe that lymphatic drainage would strengthen the immune system.
In people suffering from pneumonia, this type of massage would also help relieve pain and muscle tension in the chest13. In addition, it would promote the evacuation of pulmonary secretions.
See our Lymphatic Drainage sheet.
Written by: Dr. Dominic LaroseCardiologistDecember 16, 2021, at 10:35 a.m.