Do you know type 1 diabetes? Do you think you have it?
Then consult all the information gathered in our sheet.
Type 1 diabetes, what is it?
Type 1 diabetes accounts for 5-10% of all diabetes cases. This form of the disease most often appears during childhood or adolescence, hence its old name of “juvenile diabetes”.
At the very beginning, type 1 diabetes does not cause any symptoms because the pancreas remains partially functional. The disease only becomes apparent when 80-90% of the pancreatic insulin-producing cells are already destroyed.
Indeed, individuals with type 1 diabetes produce very little or no insulin at all due to an autoimmune reaction that partially or completely destroys beta cells in the pancreas. The latter have the role of synthesizing insulin, which is essential for the use of blood glucose by the body as a source of energy.
In this type of diabetes, it is absolutely necessary to take insulin regularly, hence the name that is often attributed to it “insulin-dependent diabetes (IDD)”. Moreover, this disease was fatal before it was possible to control it with insulin.
Type 1 diabetes: the causes of the disease
It is not known what precisely causes the immune system to react to beta cells. Some individuals are predisposed to the disease, by their heredity. A family history of type 1 diabetes is found in just under 10% of cases.
It is likely that the disease results from a combination of genetic and environmental factors. Exposure to certain viruses or foods early in life could, for example, play a role in the onset of the disease.
Type 1 diabetes: possible complications
For information on acute complications (hypoglycaemia and hyperglycaemia caused by treatment adjustment; ketoacidosis in untreated diabetics), consult our Diabetes (overview) fact sheet.
In the long term, type 1 diabetes increases the risk of several health problems: cardiovascular disease, kidney problems, loss of sensitivity in the fingers and feet, vision problems that can go as far as blindness, etc.
The best way to prevent these complications is to regularly monitor blood sugar, blood pressure and cholesterol. For more information, see our Complications of Diabetes fact sheet.
Watch out for celiac disease
Celiac disease is particularly common in people with type 1 diabetes: 20 times more than in the general population, according to one study .
Celiac disease is another autoimmune disease whose symptoms (mainly digestive) are triggered by the consumption of gluten, a protein contained in several cereals.
Therefore, screening for celiac disease is recommended in type 1 diabetics, even in the absence of obvious symptoms.
The symptoms of type 1 diabetes are numerous.
To know them, consult our complete and detailed file on this subject below.
Type 1 diabetes: symptoms
- Excessive elimination of urine (it is common to get up at night to urinate);
- increased thirst and hunger;
- significant fatigue;
- weight loss;
- blurred vision.
| Remark. More frequent infections, slower healing of wounds, or loss of feeling in the feet are some of the possible signs of complications. It is then necessary to consult your doctor without delay. See also our Diabetes Complications sheet. |
Some people are more at risk of developing type 1 diabetes. Also, risk factors favor its appearance.
Discover them here.
Type 1 diabetes: people at risk
People with a hereditary predisposition (a family history). When a close relative has type 1 diabetes (father, mother, brother or sister), the risk of also having it varies between 5% and 10%. In identical twins, when one of the two is affected, the other develops the disease in 30% to 50% of cases 1 .
As epidemiological studies indicate, type 1 diabetes is more common in populations living far from the equator. Thus, in Finland, the disease is 2 to 3 times more frequent than in the United States, and 400 times more than in Venezuela . An insufficient intake of vitamin D, the production of which depends on exposure to the sun, could partly explain this phenomenon.
type 1 diabetes: risk factors
There is no established risk factor. Here are some assumptions.
Cow milk
Early consumption of cow’s milk in infants may contribute to the onset of allergies and type 1 diabetes in children with a family history of diabetes3.
Public health authorities also advise not to give cow’s milk to newborns before the age of 12 months. Type 1 diabetes is rarer in individuals who have been breastfed.
Early introduction of cereals
Too early introduction of cereals (before the age of 4 months) could contribute to the disease; do not give it to the baby before the age of 6 months.
Respect the recommended age for introducing food to a baby.
Viral infection
An infection with Epstein-Barr virus, Coxsackie virus or cytomegalovirus, for example, could trigger the autoimmune reaction against the pancreas.
Some preventive measures can be put in place to prevent the onset of type 1 diabetes.
Discover them in this sheet.
Type 1 diabetes: preventive measures
Basic preventive measures
To prevent type 1 diabetes, it would be necessary to prevent the destruction of the cells of the pancreas responsible for the production of insulin in individuals at high risk of having the disease.
According to the Canadian Diabetes Association, there is still no effective and safe method to prevent this disease, even if we consult very early in the life of a child considered at risk.
Consequently, any approach aimed at preventing type 1 diabetes will have to be done in close collaboration with a physician and, in some cases, within the framework of an experimental study 4 .
Current research
Vitamin D
Several observational studies have shown that vitamin D supplementation of young children significantly lowers the risk of developing type 1 diabetes (daily dosages range from 400 IU to 2000 IU)13.
However, no clinical trial has yet confirmed this11. Given the lack of risks associated with taking vitamin D and its many health benefits, some doctors recommend it as a preventive measure.
Immunotherapy
This is the most promising path, and the one in which scientists are investing the most. Immunotherapy aims to allow the immune system to « tolerate » the cells of the pancreas responsible for the production of insulin.
Several forms of immunotherapy are being tested, for example5:
- a vaccine composed of antigens from the pancreas of the person to be treated;
- an autologous immune cell transplant.
This autograft would make it possible to remove the destructive cells and allow the development of new tolerant cells and the transfusion of blood taken from the umbilical cord at the time of birth (in young children).
Vitamin B3
In vitro data and animal trials have supported the hypothesis that niacinamide (vitamin B3) may have a protective effect on pancreatic beta cells. A few preliminary clinical trials have also nurtured this hope6.
However, larger studies have not yielded convincing results. For example, in the European Nicotinamide Diabetes Intervention Trial (ENDIT)7, high doses of niacinamide or a placebo were given to 552 people at risk of type 1 diabetes (close relative affected, presence of autoantibodies against pancreas and normal glucose tolerance test). Niacinamide did not reduce the risk of developing diabetes.
Injection of low doses of insulin
One of the preventive approaches tested consists of administering small doses of insulin to people at risk. This approach was evaluated in the Diabetes Prevention Trial – Type 18.9.
Insulin therapy had no preventive effect, except in a high-risk subgroup, in whom the onset of diabetes was slightly delayed.
One of the challenges in research is to target the people most likely to develop the disease. The appearance in the blood of antibodies against the beta cells of the pancreas (autoantibodies) is one of the indicators studied.
These antibodies can be present years before the onset of the disease. Since there are several types of these antibodies, it is a question of discovering which are the most indicative of the disease, and from what quantity .
Measures to prevent complications
See our Diabetes Complications fact sheet.
In the case of type 1 diabetes, certain treatments and complementary approaches make it possible to treat the disease effectively.
Check out the full list below.
Type 1 diabetes: medical treatments
Diabetics can hope to lead an active, independent and dynamic life provided they respect, throughout their lives, strict discipline by:
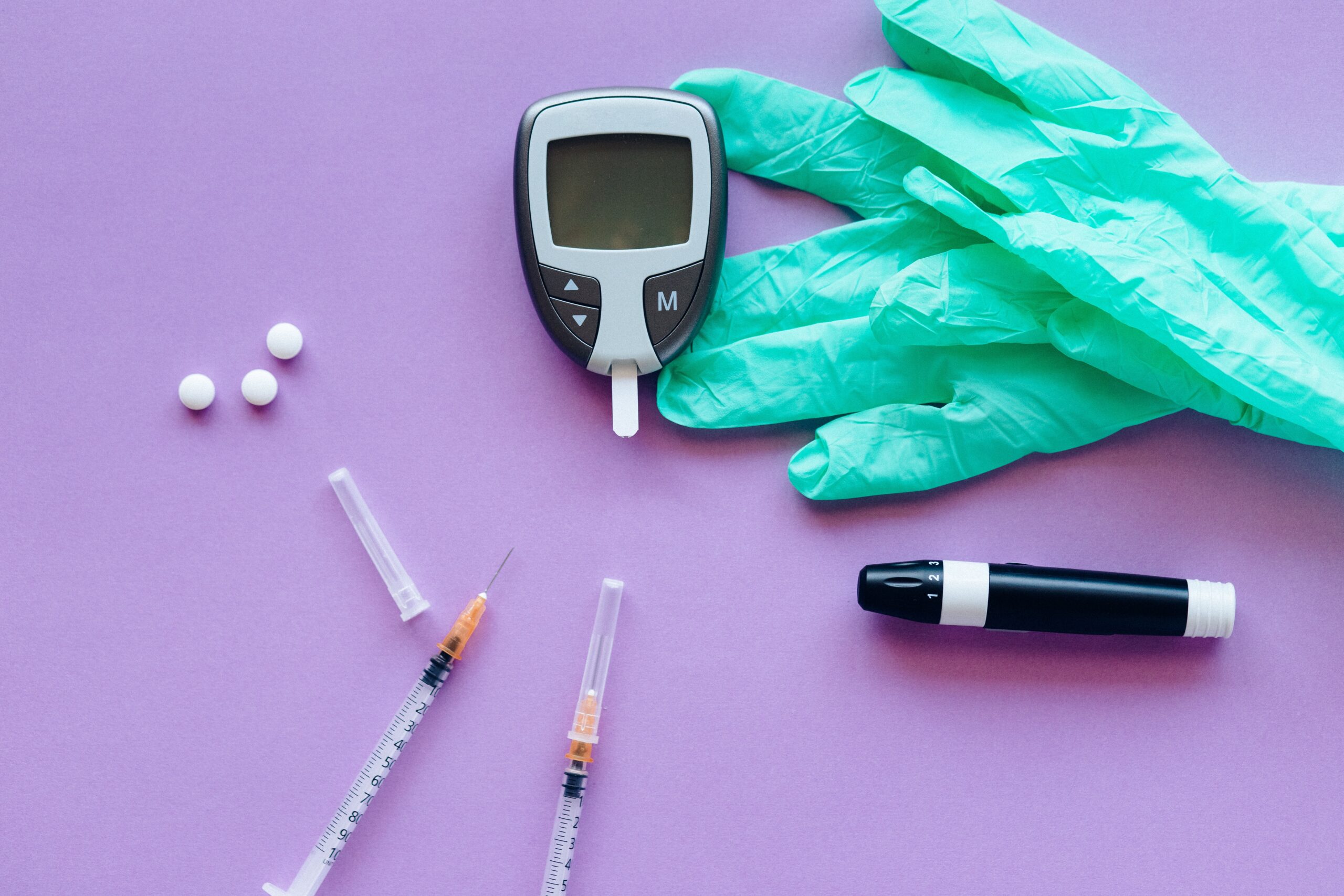
- monitoring blood glucose levels using a blood glucose meter;
- an appropriate diet;
- a physical exercise program.
In our Diabetes fact sheet (overview), you will find:
- a diagram of glucose uptake;
- a table of blood glucose values for adolescents and adults with diabetes;
- a diet plan;
- physical exercise suggestions;
- ways to better manage stress.
People with type 1 diabetes often need to be treated for health problems that may be associated with this disease.
Medication
People with type 1 diabetes must inject insulin to compensate for the insufficiency of the pancreas to produce it. Injecting rather than taking insulin by mouth is necessary because it is destroyed by digestive juices. As the treatments are daily (often several times a day), the patient must learn to administer the injections himself.
The dosage and the type of insulin used vary according to the actual insulin needs of the subject, at each moment of the day. Hence the need for close medical monitoring. At the start of treatment, it may take some time to find the right dosage.
There are different types of insulin, with different speeds of action. The majority of patients practice 3 to 5 injections per day, or use an « insulin pump », a small device installed on the body and designed to provide a continuous infusion of insulin 24 hours a day. The goal is to ensure, at all times, that blood sugar levels are as close to normal as possible.
In this way, the incidence and severity of complications associated with type 1 diabetes are significantly reduced. Long-acting insulins, which require a single injection per day, are also available. The choice of insulin type should be made with the attending physician.
Surgery
In recent years, researchers have been increasingly interested in the therapeutic benefits of pancreas or islets of Langerhans transplantation in type 1 diabetics.
Because of the risks, pancreas transplantation is reserved for cases where diabetes cannot be controlled by insulin injections or in case of serious complications.
Less expensive and less risky, the transplantation of islets of Langerhans is still at the experimental stage.
Type 1 diabetes: complementary approaches
Certain natural products can help prevent complications associated with type 1 diabetes.
See our Diabetes Complications fact sheet.
As part of its quality approach, Passeportsanté.net invites you to discover the opinion of a health professional.
Dr. Dominic Larose, emergency physician, gives you his opinion on type 1 diabetes.
Type 1 diabetes: the opinion of Dr. Dominic Larose
« In the past, type 1 diabetes caused death shortly after diagnosis, once the symptoms set in. Today, insulin saves life. But the repercussions on daily life, as well as the constraints related to the disease and its treatment are often very heavy to bear for the patient and his family.
A patient who is extremely well informed about his disease is the sine qua non of success in order to live the best possible life. It also helps to overcome the disadvantages attached to it.
The family must also become an expert in the matter. The patient will benefit greatly from the help offered by the multidisciplinary diabetes team. »
Dr Dominic Larose, M.D.
Do you know type 1 diabetes? Do you think you have it?
Then consult all the information gathered in our sheet.
Type 1 diabetes, what is it?
Type 1 diabetes accounts for 5-10% of all diabetes cases. This form of the disease most often appears during childhood or adolescence, hence its old name of “juvenile diabetes”.
At the very beginning, type 1 diabetes does not cause any symptoms because the pancreas remains partially functional. The disease only becomes apparent when 80-90% of the pancreatic insulin-producing cells are already destroyed.
Indeed, individuals with type 1 diabetes produce very little or no insulin at all due to an autoimmune reaction that partially or completely destroys beta cells in the pancreas. The latter have the role of synthesizing insulin, which is essential for the use of blood glucose by the body as a source of energy.
In this type of diabetes, it is absolutely necessary to take insulin regularly, hence the name that is often attributed to it “insulin-dependent diabetes (IDD)”. Moreover, this disease was fatal before it was possible to control it with insulin.
Type 1 diabetes: the causes of the disease
It is not known what precisely causes the immune system to react to beta cells. Some individuals are predisposed to the disease, by their heredity. A family history of type 1 diabetes is found in just under 10% of cases.
It is likely that the disease results from a combination of genetic and environmental factors. Exposure to certain viruses or foods early in life could, for example, play a role in the onset of the disease.
Type 1 diabetes: possible complications
For information on acute complications (hypoglycaemia and hyperglycaemia caused by treatment adjustment; ketoacidosis in untreated diabetics), consult our Diabetes (overview) fact sheet.
In the long term, type 1 diabetes increases the risk of several health problems: cardiovascular disease, kidney problems, loss of sensitivity in the fingers and feet, vision problems that can go as far as blindness, etc.
The best way to prevent these complications is to regularly monitor blood sugar, blood pressure and cholesterol. For more information, see our Complications of Diabetes fact sheet.
Watch out for celiac disease
Celiac disease is particularly common in people with type 1 diabetes: 20 times more than in the general population, according to one study .
Celiac disease is another autoimmune disease whose symptoms (mainly digestive) are triggered by the consumption of gluten, a protein contained in several cereals.
Therefore, screening for celiac disease is recommended in type 1 diabetics, even in the absence of obvious symptoms.